1)Primary Liver Cancer
Malignant tumors (cancer) that develop in the liver are collectively called “primary liver cancer.” Liver cancer usually refers to primary liver cancer and not metastatic liver tumor or liver metastases. (See details of metastastic liver tumors here)。
①Hepatocellular Carcinoma (HCC)
About 95% of primary liver cancers are hepatocellular carcinoma that derives from liver cells (hepatocyte). Hepatocellular carcinoma (HCC) usually occurs in the “damaged liver” caused by hepatitis B, hepatitis C, heavy alcohol consumption, fatty liver, etc., and rarely occurs in patients with normal liver. The relative survival rate of cancer in Japan is shown below (based on data from the National Cancer Center Cancer Information Service).
| 5-year survival | 10-year survival | |
| Colorectal Cancer | 76.8% | 67.8% |
| Gastric Cancer | 74.9% | 65.3% |
| Lung Cancer | 45.2% | 30.9% |
| Liver Cancer | 37.0% | 15.6% |
| Biliary Cancer | 28.6% | 18.0% |
| Pancreatic Cancer | 9.9% | 5.3% |
(data from the National Cancer Center Cancer Information Service)
The prognosis of hepatobiliary cancers is generally poor. Although hepatocellular carcinoma has various treatment options, the reason why hepatocellular carcinoma is classified as poor-prognosis cancers depends on its mechanism of development. Cancers such as gastric cancer and colorectal cancer can be completely cured by treatment such as surgery at an early stage, and it is basically judged to be “cured” when no recurrence is confirmed in 5 years from curative resection. However, in the case of hepatocellular carcinoma, the damaged liver is a hotbed for producing cancer one after another, so even if the cancer that is currently visible can be completely resected, new cancers may occur at a certain frequency over time. Since the liver, which once became the origin of cancer, cannot be recovered by treatment, it is unlikely that hepatocellular carcinoma can be cured with a single treatment, and regular lifelong checks for recurrence are required.
②Intrahepatic Cholangiocarcinoma (ICC)
Intrahepatic cholangiocarcinoma (ICC) is the second most common type of primary liver cancer after hepatocellular carcinoma. Intrahepatic cholangiocarcinoma is cancer that derives from the cells of intrahepatic bile duct. Intrahepatic cholangiocarcinoma is a relatively rare cancer that occurs not only in damaged liver but also in normal liver, and frequently detected in advanced stages because it is difficult to predict who is likely to develop intrahepatic cholangiocarcinoma and there are few effective treatments except for surgery.
③Other rare hepatic malignancies
Other rare primary liver cancers include cystadenocarcinoma, malignant lymphoma, neuroendocrine tumor, angiosarcoma, and epithelioid hemangioendothelioma. These tumors are quite rare and there is no standardized treatment. Surgical treatment is basically performed, but in some cases additional medical treatment (e.g., chemotherapy for malignant lymphoma) is required. Therefore, it is desirable to receive treatment at a specialized hospital for cancer.
2)Treatment for Hepatocellular Carcinoma
The treatment for hepatocellular carcinoma is determined by “size”, “number”, “location”, and “liver function”. This is called “standard treatment”. Standard treatment means the “currently most effective” treatment established by various clinical studies by physicians around the world, and does not mean “ordinary” treatment. New treatments with unknown or little evidence are offered in the form of “clinical trials” or “advanced medical care”, but unfortunately there is no scientific basis for other treatments.
In relatively early stage liver cancer, there are cases where several treatment methods can be selected depending on the tumor conditions. However, because each treatment method has its strengths and weaknesses and the malignant potential of the same cancer varies from person to person, it is important to choose optimal treatment options according to each patient’s clinical status.
Unfortunately, hepatocellular carcinoma recurs at relatively high rate even after curative-intent treatment for early stage cancers. Thus, it is important to select treatment in anticipation of treatment options in the event of recurrence. Experience and skill are required in surgery for hepatocellular carcinoma, as treatment must avoid procedure that potentially make the next surgery impossible or technically highly demanding. Because the long-term survival probability of hepatocellular carcinoma is significantly dependent on the choice of treatment, it is essential to determine optimal treatment options in multidisciplinary discussions in medical team (Shindoh J, et al. J Gastrointest Surg 2020)。
Regarding the basics of treatment selection, the treatment algorithm of the liver cancer clinical practice guideline published by the Japanese Society of Hepatology is shown below.

3)Our Surgical Indication
⓪Premise
First of all, the main premise of surgery is that it is technically feasible and oncologically acceptable. Surgery is indicated for cases where i) there is a physical condition that can withstand the surgery, ii) technically complete resection is expected to be possible, and iii) surgery is considered to be meaningful basically depending on the above guidelines. Regarding iii), the idea is almost the same at all institutions, while the idea may differ depending on the institutions regarding i) and ii) due to differences in the experience and skills of the surgeon and the indication criteria for surgery. If you are not satisfied with the treatment offered or have any questions for the other treatment options, we recommend that you get a second opinion.
①Solitary lesion
Hepatectomy is the first-line treatment for solitary hepatocellular carcinoma, and ablations (such as radiofrequency ablation (RFA)) is recommended as the second-line treatment for cases with a tumor measuring up to 3 cm. Both surgery and ablations are performed with a curative intent, but the larger the tumor diameter, the more difficult the treatment becomes. Recently, increasing number of cases have successfully undergone laparoscopic resection. However, even when choosing laparoscopic resection, the first priority is the safety of surgery, and not all surgery can be performed laparoscopically even for a single tumor.
②Multiple lesions
For up to 3 tumors, resection or ablations is recommended for tumors with a diameter of 3 cm or less, and resection or transcatheter arterial chemoembolization (TACE) is recommended for cases larger than 3 cm. Since multiple tumors increase the risk of recurrence after treatment, the appropriate treatment should be selected for each individual case. In cases where the number of tumors exceeds 4, it is difficult to cure by resection or ablations, and TACE or chemotherapy is basically selected.
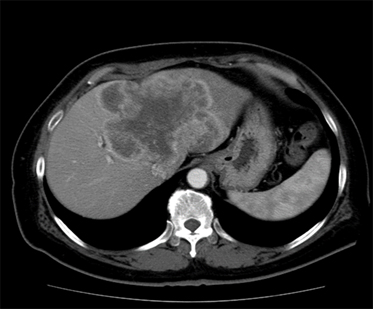
③Tumors with major vascular invasion
Hepatocellular carcinoma easily invades blood vessels such as portal veins and hepatic veins, and it breaks through the blood vessel wall and begins to grow inside the lumen of the blood vessels (tumor thrombus). Although such advanced hepatocellular carcinoma has poor prognosis, out team has many experiences with aggressive treatment for advanced hepatocarllular carcinoma and favorable outcomes have been achieved.
④Treatment of extrahepatic metastases
Metastasis of hepatocellular carcinoma is common in the lymph nodes, adrenal glands, lungs, bones, and peritoneum. Patients with extrahepatic disease are usually not a candidate for curative resection. However, surgical resection is thought to be effective in selected cases. At out institution, surgery is selected for patients who respond well for systemic/locoregional therapies as a part of multidisciplinary treatment.
⑤Hepatocellular carcinoma with poor hepatic function
Child-Pugh C patients are not eligible for resection and may be indicated for liver transplantation depending on the tumor conditions. Our team uses a unique criteria for maximum extent of surgery for patients with severe hepatic injury(Kobayashi Y, Shindoh J, HPB 2019), and zero mortality has been achieved in initial hepatectomy for patients with severe hepatic injury (incl. Child-Pugh C) and portal hypertension.
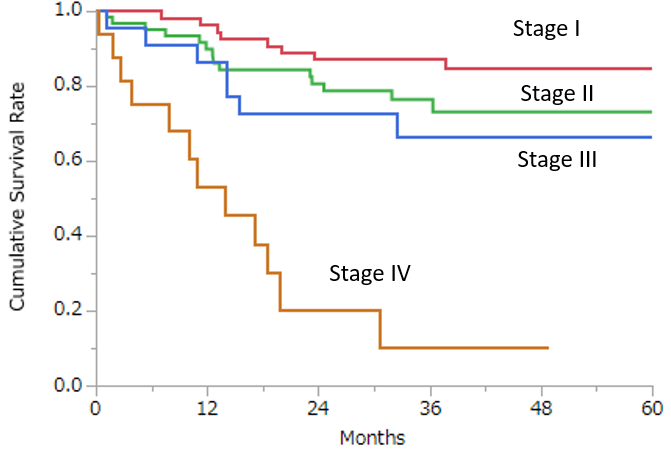
Here is a summary of my personal series of initial hepatectomy for hepatocellular carcinoma (2014-2017, n=156). Median size of tumor was 32mm (range, 4-180mm), 28.2% of the patients presented multiple lesions, 12% of patients were Child-Pugh B, median value of indocyanine green retention rate at 15 minutes was 17.7% (range, 1.5-62.4%), and 44.9% of patients were cirrhotic. Overall survival rates at 1-year, 3-year, and 5-year were estimated as 88.2%, 72.1%, and 71.0%, respectively for the entire population (median observation period, 39.4 months). Survival outcomes of each stage were shown in the Figure. Approximately 10% points superiority have been maintained in survival outcomes compared to those reported in Japanese nationwide survey in 2013.